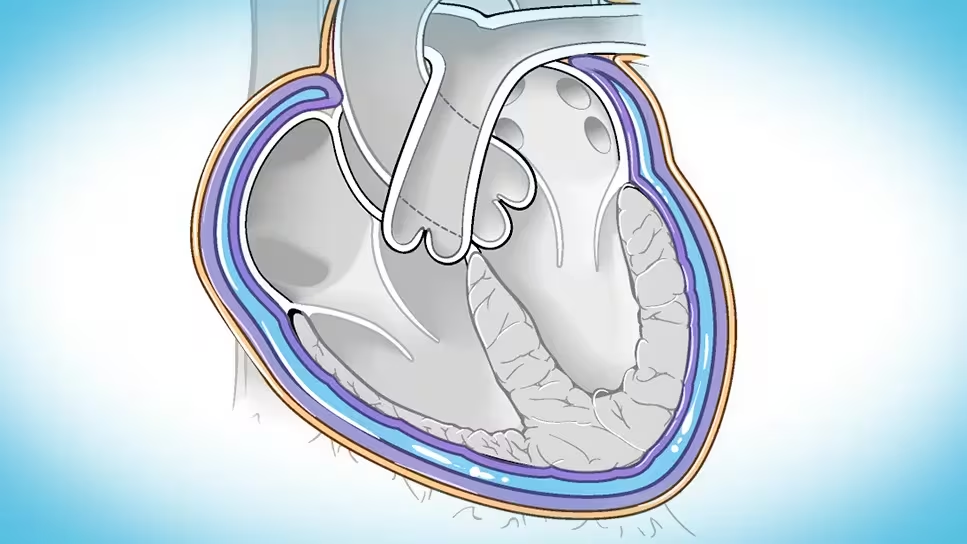
Pericarditis is the inflammation of the thin sac surrounding the heart, called the pericardium. It can be acute and short-lived, last several weeks, or even become chronic. The condition may present with chest pain, fluid build-up around the heart, or serious complications like cardiac tamponade (where pressure from fluid prevents the heart from beating properly).
In Uganda, most cases are caused by viral infections, but other infections, autoimmune reactions, kidney failure, and even trauma can also trigger it.
If you are experiencing chest pain that worsens when breathing deeply or lying down, you can get timely advice and support through Hope Plus. This service connects you with licensed doctors who can guide you on treatment and follow-up.
Key Takeaways
- Pericarditis is inflammation of the membrane covering the heart.
- Common causes include viral infections, bacterial infections like TB, and complications of heart attack or kidney failure.
- Symptoms include sharp chest pain, muffled heart sounds, and in severe cases, life-threatening cardiac tamponade.
- Diagnosis is done using ECG, chest X-ray, and echocardiogram.
- Treatment usually includes rest, anti-inflammatory medicines (such as ibuprofen), and removal of fluid if necessary.
Causes
- Viral infections (most common): Coxsackie A & B, influenza, varicella
- Bacterial infections: tuberculosis, staphylococcus, streptococcus, meningococcus, pneumococcus, gonococcus, mycoplasma
- Fungal infections: histoplasmosis (rare)
- Other causes:
- Severe kidney failure (uraemia)
- Autoimmune reactions (rheumatic fever, hypersensitivity)
- Heart attack (post-myocardial infarction syndrome)
- Radiation therapy
- Trauma or injury to the chest
- Cancers affecting the heart covering (neoplasms)
Symptoms and Clinical Features
- Pericarditis without fluid (effusion): sharp retrosternal pain radiating to the shoulder, worsened by breathing, movement, or lying flat. Pain may improve when sitting up. A “pericardial rub” (a scratching sound heard with a stethoscope) is a key sign.
- Pericardial effusion (fluid around the heart): muffled heart sounds, enlarged heart silhouette on imaging, and reduced heartbeat strength.
- Cardiac tamponade (serious complication): shortness of breath, restlessness, low blood pressure, rapid pulse, weak heart output, and pulsus paradoxus (blood pressure drops sharply when breathing in).
Differential Diagnosis
- Other causes of chest pain (heart attack, pulmonary embolism, gastritis, peptic ulcer)
- Other causes of heart failure (dilated cardiomyopathy, severe valvular disease)
Investigations
- ECG: may show characteristic changes such as widespread ST elevation
- Chest X-ray: to check heart size or fluid build-up
- Echocardiography (Echo): best for detecting pericardial effusion and tamponade
Treatment
If viral or idiopathic pericarditis
- Rest
- Ibuprofen 600 mg every 8 hours for pain and inflammation
- Close monitoring for complications
If there is fluid (pericardial effusion)
- Pericardiocentesis (tapping the fluid) if large or causing tamponade
If secondary to other causes
- Treat the underlying cause:
- TB pericarditis → anti-tuberculosis therapy
- Kidney failure → dialysis
- Bacterial infections → antibiotics
- Cancer-related → oncology-directed care
Prevention
- Early treatment of infections like TB, pneumonia, and rheumatic fever
- Regular monitoring for patients with kidney failure
- Quick medical attention for chest pain that changes with breathing or body position
Frequently Asked Questions
Is pericarditis life-threatening?
Most cases are mild and recover with rest and medicine, but if fluid builds up quickly around the heart, it can be life-threatening.
How can I tell pericarditis pain apart from a heart attack?
Pericarditis pain is sharp, worsens with breathing or lying down, and may improve when sitting forward. Heart attack pain is usually heavy, crushing, and not affected by position.
Can pericarditis come back?
Yes. Some people may experience recurrent or chronic pericarditis, especially if the cause is autoimmune or not fully treated.
When should I see a doctor?
Seek care urgently if you have severe chest pain, fainting, shortness of breath, or swelling of the abdomen or legs.