Cryptococcal meningitis (CM) is a serious fungal infection caused by Cryptococcus neoformans. In Uganda, it can be life-threatening, with mortality rates up to 39%. People with a CD4 count below 100 cells/µL are at the highest risk, making early screening and proper management essential.
If you are living with HIV, understanding your risk and what to do if you develop symptoms is critical. Through Hope Plus, you can get personalised guidance from licensed doctors who help you understand your health, explain test results, and advise on when to seek urgent care. This support ensures you know the right steps to protect yourself.
Who Should Be Screened
- ART-naive individuals with CD4 <100 cells/µL
- Patients on ART with viral load >1000 copies/ml or signs of treatment failure
Screening is done using the cryptococcal antigen (CrAg) test, a simple bedside finger-prick test. Early detection allows for timely care and reduces the risk of severe illness.
What Happens After Screening
- If CrAg is negative and there are no meningitis symptoms: Start ART immediately or adjust your regimen if needed.
- If CrAg is positive or symptoms of meningitis are present (headache, seizures, confusion, stiff neck, sensitivity to light):
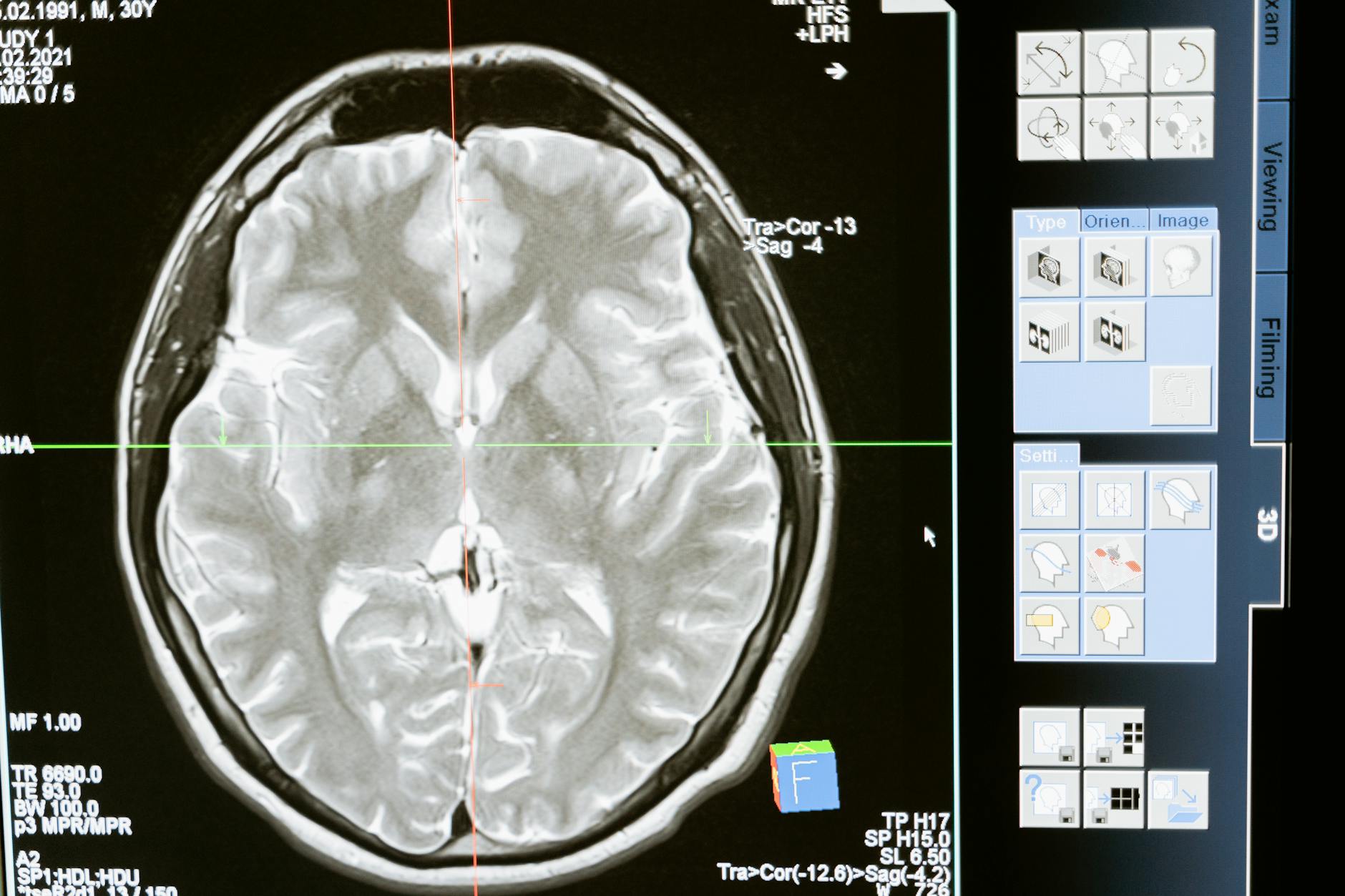
- A lumbar puncture (LP) is performed to test cerebrospinal fluid (CSF).
- If CSF CrAg is positive, treatment for cryptococcal meningitis is initiated.
- If CSF CrAg is negative but blood CrAg is positive, pre-emptive treatment for asymptomatic cryptococcal disease is started.
Timing of ART
- ART is usually delayed 4–6 weeks after starting CM treatment to reduce complications from immune reconstitution.
- People already on ART may have adjustments or temporary pauses depending on adherence and prior resistance. Your healthcare provider will guide the safest approach.
Managing Cryptococcal Meningitis
Induction Phase (2 weeks)
- High-dose Amphotericin B + Flucytosine + Fluconazole, or alternative regimens depending on availability
- Monitoring for kidney problems and electrolyte imbalances is important
Consolidation Phase (8 weeks)
- Fluconazole at a lower dose to support recovery
- ART is started 4–6 weeks after beginning antifungal therapy
Maintenance Phase (18 months)
- Fluconazole continues to prevent relapse
- Treatment can stop once CD4 counts improve and viral load is suppressed
Relapse and CSF Pressure Management
- Recurrence of meningitis symptoms requires testing for drug resistance.
- High cerebrospinal fluid pressure is managed with therapeutic lumbar punctures, which can improve survival by 25%.
Key Takeaways
Cryptococcal meningitis is a medical emergency for people living with HIV, but early screening, careful monitoring, and timely management can save lives. Regular CD4 and viral load checks, along with awareness of warning symptoms, are essential.
For guidance on understanding your risk, interpreting test results, and knowing what steps to take, connect with licensed doctors through Hope Plus. They provide personalised advice and help you navigate your care confidently.